[vc_row][vc_column][vc_column_text]It probably won’t shock you to know the best practices for giving CPR and defibrillation differ if you’re giving them to a younger person or a fully grown adult.
However, it may surprise you to learn, that some of those important guidelines differ greatly, even between those two treatments.
It’s incredibly important to understand the guidelines for both, because 12 otherwise healthy young people in the UK die suddenly each week from heart-related problems.
So while we’ve explored the basics of defibrillation and CPR on adults in past blogs, here, we’ll look at how to effectively use both CPR and defibrillation on children and infants.
How to safely use CPR on children and infants
[/vc_column_text][vc_empty_space][vc_single_image image=”2492″ img_size=”full”][vc_empty_space][/vc_column][/vc_row][vc_row][vc_column][vc_column_text]For CPR, Resuscitation Council UK defines a child as being aged between one and 18 years, and an infant as under one year old. (It also gives special labels to a baby under one month old – a neonate – and a baby just after birth – a newborn).
The guidance for giving CPR to infants and children is as follows:
- Check they are responsive by shaking their shoulders and shouting loudly in both ears
- Check their breathing by observing chest movement, listening for breath and feeling for their breath on your cheek. If they are not breathing, or are breathing erratically, check for an obstruction in the mouth or throat. (This is the cause of breathing problems in children far more than in adults!).
- Shout for help and start CPR immediately, giving 30 chest compressions at 4cm deep with two fingers for a newborn or infant, or 5cm with one or both hands for a child up to 18 years old depending on their size. Then give two rescue breaths (unless following current Covid-19 CPR guidelines).For a child over one year old, tilt the head back and lift the chin to expose the airway before closing their nose gently with your finger and thumb. Blow into their mouth for around one second, watching for their chest rising. Give two rescue breaths in total.For an infant under one year old, do the same without tilting their head back, and covering both the baby’s mouth and nose with your mouth.Do the above for one minute, then…
- Call 999 and request an ambulance to arrive urgently
- Continue the CPR process, alternating between 30 compressions and two rescue breaths until the ambulance arrives
- If you are worried about giving rescue breaths (possibly due to Covid-19 or otherwise), continue with chest compressions only.
These are the basics of how to perform CPR on children and infants – but they are only a primer. For more details, see Resuscitation Council’s advanced paediatric life support guidelines or alternatively the NHS guidelines on how to resuscitate a child.
How to safely use defibs on children and infants
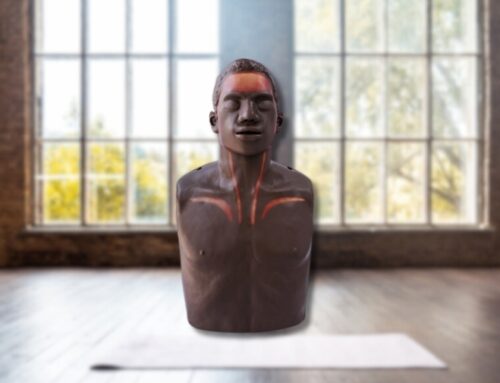
[/vc_column_text][vc_empty_space height=”16px”][vc_empty_space height=”16px”][vc_row_inner][vc_column_inner width=”1/2″][vc_column_text]One of the most popular questions we get asked on this topic is ‘Do you use a defibrillator on a child?’
The answer is yes – albeit ideally at lower power (of 50-75 joules) than a typical adult-suggested defibrillator voltage (which starts as standard at 150 joules). This can be done by using an AED that has either paediatric pads that adjust the energy output, or a built-in paediatric attenuator like the iPAD SP1. If the defibrillator doesn’t have an attenuator or child pads, or if you are unsure about whether it does, don’t delay; deliver a shock using the standard AED as it comes. Each moment without defibrillation during a sudden cardiac arrest lowers survival chances by 10%.
(Remember, an AED will not advise or allow you to shock someone whose heart does not have a shockable rhythm – meaning you cannot hurt someone mistakenly using an AED).[/vc_column_text][/vc_column_inner][vc_column_inner width=”1/2″][vc_single_image image=”2493″ img_size=”full”][/vc_column_inner][/vc_row_inner][vc_empty_space height=”16px”][vc_column_text]It’s important to note that one of the main differences between CPR and defibrillation guidelines is that with defibrillation, a child is considered to be anyone aged between one year and up to eight years old. Anyone eight years old or above is treated as an adult when it comes to reviving them using an automated external defibrillator (AED). A baby below one year old is considered an infant.
To use a defibrillator on a child or infant under eight years old:
- First, start CPR as directed above
- If there is more than one rescuer, the second one should call 999 and locate an accessible AED if one is nearby
- If an AED is available, apply the defibrillator pads to the casualty while the first rescuer continues to give CPR.
- For children, attach the AED pads to the upper right chest and lower left chest, the same as with an adult. For an infant, place one pad on the front of the chest and the other on the back
- The AED will scan the casualty’s heart and determine if it is suitable to administer a shock. If it is, depending on the AED’s settings it will either administer the shock automatically, or prompt you to do so by pressing the shock button
- If there is no change, the AED will prompt you to continue the cycle of CPR and shocks until an ambulance arrives, at which point first responders will take over looking after the patient.
For more details on how to safely use defibs on children and infants, see Resuscitation Council’s advanced life support guidelines, or alternatively this AED guide for schools by the NHS’s South Central Ambulance Service.
Should you use child defib setting if the child is adult-sized?
Yes. Unlike with CPR, the size of the child has no bearing on the treatment given when it comes to defibrillation. With CPR, the child or infant’s size directly affects the amount of pressure you put on their chest to keep the heart pumping. In other words, CPR effectively treats the heart through external pressure. Defibrillation treats the heart internally by resetting the sinoatrial node, so what matters is the age and the maturity of the heart – not its physical dimensions.
So, whether dealing with a child who’s bigger than many fully-grown adults, or an adult who is smaller than most, follow the appropriate defibrillation guidelines above factoring in age, rather than size.
Do you know where your nearest defibrillator is?
If not, the National Defibrillator Database can help in a hurry.
No defibrillator near where you live, work or enjoy your leisure time? Then you might want to look into getting your own!
To understand which defibrillator might be best for you, visit our guide to choosing the right defibrillator or get in touch to discuss your options in person.[/vc_column_text][vc_empty_space][/vc_column][/vc_row][vc_row][vc_column][vc_column_text]
Related articles
- Choosing the Right Defibrillator
- What Happens When You Use A Defibrillator?
- World Heart Day: Heart Attack or Cardiac Arrest?
- World First Aid Day: CPR Guidance in a Covid-19 World
- Defibrillator Myths Busted
[/vc_column_text][/vc_column][/vc_row]